Trigeminal
Neuralgia Treatment Center of Virginia
A Patient’s Guide to Understanding of TN

A GUIDE TO
USING THIS BOOKLET
This booklet is designed to give you the patient a brief
education about trigeminal neuralgia and the treatments
offered through Dr. K. Singh Sahni. We have tried to explain
difficult terms and concepts in lay terms. For instance,
you will find unfamiliar medical terms in bold italics
explained within the text and in the glossary that follows.
Of course, this information is by no means exhaustive
or all-inclusive, and you are encouraged to discuss any
specific concerns or questions with your surgeon.
TRIGEMINAL
NEURALGIA
Trigeminal Neuralgia (TN), also known as tic
douloureux, has been described as one of the most painful
human afflictions. It has been compared to severe toothache
or even labor pain. The pain is usually sharp and shooting
and is very episodic and intermittent. It involves the
trigeminal nerve which provides sensation to the face,
teeth, mouth and nose. In most but not all patients, symptoms
can be triggered by touching the face, brushing the teeth,
feeling a breeze of air, putting on makeup, shaving, or
merely touching certain parts of the face.
There is no specific
test that can identify trigeminal neuralgia, so the best
method of diagnosis is to obtain a good history from the
patient. About two percent of trigeminal neuralgia patients
harbor a tumor or some other sort of mass compressing
the trigeminal nerve. Some of the most common causes are
believed to be:
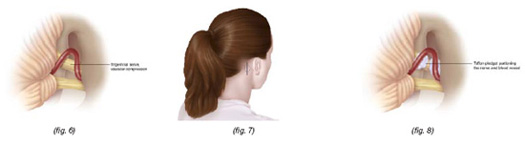
• Vascular
compression in which a blood vessel causes compression
on the trigeminal nerve in the region very close to the
brain stem called the root entry zone. (fig. 6)
• Multiple
sclerosis (MS), While trigeminal neuralgia is usually
found in patients over the age of 50, multiple sclerosis
patients are usually younger than the average TN patient
and may have bilateral (two sided) facial pain. Every
young person with trigeminal neuralgia does not necessarily
have MS.
A physician experienced
in the management of trigeminal neuralgia can often make
the appropriate diagnosis in a single interview.
The trigeminal nerve,
also known as the fifth cranial nerve, has three branches:
1. Ophthalmic (around
the eye);
2. Maxillary (around the upper jaw);
3. Mandibular (around the lower jaw).
The pain may be limited
to one or more of these branches. In fact, many categorize
the pain as atypical if it spreads beyond the distribution
of the trigeminal nerve. For example, pain going down
to the neck, shoulder, on top of or behind the head would
not be coming from the trigeminal nerve. Trigeminal neuralgia
involves attacks of severe pain on the affected side of
the face and is rarely bilateral. The sharp attack may
last just for a few seconds, but in advanced cases these
attacks could last much longer. As mentioned above, the
exception to this rule is the multiple sclerosis patient
who may suffer from bilateral facial pain.
TREATMENT
OPTIONS
Medications
In general, the first line of treatment for trigeminal
neuralgia is medical. Anticonvulsants are frequently used
for medical treatment of trigeminal neuralgia. For the
majority of patients, these medications are quite effective.
Medical treatment
with anticonvulsants must be tailored to the patient’s
medical condition, age and general medical status including
kidney and liver function since many of these medications
may have effects with long-term use on kidney and liver
function if they are not closely monitored. Usually the
prescribing physician will closely monitor the dosage
and obtain kidney and liver functions tests as well as
blood counts for as long as these medications are taken.
Surgery
Patients unable to tolerate the medications or whose pain
has become refractory (resistant to treatment) are then
referred to a neurosurgeon with special interest and experience
with trigeminal neuralgia. The three primary surgical
options for the treatment of trigeminal neuralgia are:
Trigeminal
Glycerol Rhizolysis (TGR)
A procedure done in the hospital operat-ing room under
monitored anesthesia. The anesthesiologist will utilize
appropriate medications to decrease anxiety and help with
sedation. General anesthesia (being put to sleep) is usually
not necessary; however, intravenous medications are given
so that you will be very relaxed and sleepy. In the majority
of cases, you will not even remember the procedure. This
is called IV sedation.
After being properly
sedated, you will be placed on the operating table and
a special x-ray device will be used to help the neurosurgeon
insert the needle. The needle is advanced until it reaches
a small pocket of fluid surrounding the trigeminal nerve
(fig. 1). A special contrast (dye) is then injected which
can be easily seen on the x-ray, and this determines the
volume of fluid around the trigeminal nerve (fig. 2).
In this way, the surgeon can calculate the exact amount
of glycerol that needs to be given. This is an important
part of the procedure and we find it an extremely important
part of the process to avoid giving an overdose of the
glycerol. Once the glycerol is measured and injected into
this pocket, the needle is removed.
During this part
of the procedure, you will usually be sitting up in the
operating room after which you are transferred to a stretcher
in the same position, sitting with the chin flexed and
the head turned to the side of the procedure. The nurse
in the recovery room will help you remain in that position
for the next two hours during which time you will be closely
monitored for comfort, your pulse, blood pressure and
breathing will be closely watched.

IMPORTANT
REMINDERS ABOUT TRIGEMINAL GLYCEROL RHIZOLYSIS
Generally you will not be “put to sleep”,
but you must have nothing to eat or drink after midnight
on the night before the procedure. You may resume your
usual diet after surgery.
The area around the
needle will be numbed before insertion of the needle;
therefore, you should let your doctor know if you have
any pain.
There will be no
incision made. A band-aid will be used to cover the area
where the needle was inserted. The band-aid may be removed
the day after the procedure.
If you are taking
any blood thinners such as aspirin, Plavix, Coumadin or
any other such medications, please inform your physician
so that they can be withheld with appropriate approval
from your primary care physicians prior to the procedure.
Patients can usually
go home the same day or the day after the procedure with
a follow-up appointment to be seen back in the office
in three to four weeks.
If you are taking
any anticonvulsants, you will probably stay on the medication
as advised by your surgeon. The medication will probably
be decreased on your first follow-up appointment. Generally
about a month later you will gradually be taken off the
medications.
Notify your surgeon
immediately if you have severe headache, nausea, vomiting,
neck stiffness or fever.
Results
Some patients are completely pain-free within twenty-four
hours of the procedure while others can take as long as
three to six weeks to gain complete relief.
TGR is the preferred
surgical approach for elderly patients with some medical
issues who are in such extreme distress that they need
urgent and immediate relief.
Patients are forewarned
that there is a small risk of potential complications
including some loss of feeling or decreased sensation
of the face. If there is any numbness along the cornea
or eye, you must be extremely careful and see an eye doctor.
Your surgeon will go over the details of other potential
risks and benefits of each procedure.
Some patients may
develop fever blisters after the injection which usually
go away quickly and need only to be taken care of with
good hygiene and appropriate medications if needed.
Gamma
Knife
Gamma Knife treatment is done under the leadership of
a neurosurgeon, a team of physicists - doctors specializing
in radiation - and nurses. Gamma Knife was pioneered in
Stockholm, Sweden by Professor Lars Leksell and has been
in use for more than thirty-five years. It is actually
not a knife at all but is a term used for 201 individual
beams of focused radiation that all converge on a selected
target. While each individual beam is not very effective,
the combination of all the beams causes a biological and
structural change in the targeted tissue. Trigeminal neuralgia
is just one of the indications for Gamma Knife, which
is also used for brain tumors.
Gamma Knife for trigeminal
neuralgia is performed for patients who are not ideal
candidates for open surgery, such as patients on blood
thinners or who have other known cardiovascular problems
and patients unable or unwilling to take anticonvulsants.
Others prefer this treatment due to its relative less
invasiveness. Gamma Knife treatment is a simple,
relatively painless and quite straight- forward process
that consists of four steps:
Prior to treatment,
your surgeon will review the entire procedure with you
and risks and benefits will be discussed in great depth.
Ample opportunity will be given for any questions you
may have. given for any questions you may have. Usually,
no incisions, stitches or shaving of the head is necessary.
You will be offered to tour the Gamma Knife facility,
watch an instructional DVD and meet the nurses.
PROCEDURE
1. The Head
Frame
Placement of the frame on the head of the patient is a
very important part of the procedure (fig. 3). This frame
allows the doctor to pinpoint the target area with extremely
high accuracy. For trigeminal neuralgia patients, the
target is usually in the vicinity of the root entry zone
of the fifth cranial nerve. This is actually the area
where the trigeminal nerve originates in the brain stem.
The anesthesiologist will give a very light intravenous
sedation so that the patient will not experience any major
pain or discomfort. The majority of patients do not even
remember this part of the procedure because of the IV
sedation.
2. Imaging
You will then be taken for imaging in a wheelchair or
on a stretcher. During this part of the procedure, most
patients are awake and alert; however, patients who experience
anxiety about the MRI or CT scan can be given further
sedation so that the imaging can be carried out.
3. Treatment
Planning
 At
this point, you and up to three visitors will be able
to sit together in the pretreatment area while the surgeon
and the rest of his team work on the treatment plan.
At
this point, you and up to three visitors will be able
to sit together in the pretreatment area while the surgeon
and the rest of his team work on the treatment plan.
The process may take
up to forty minutes. Family members accompanying the patient
may feel free to bring reading or work materials with
them. There is also a television and DVD player in the
room for entertainment.
During treatment
planning, data from the images is transferred to a special,
highly sophisticated computer. Unlike gamma knife treatment
for brain tumors in which the tumor is outlined, trigeminal
neuralgia patients will have the nerve outlined in multiple
imaging sequences.
Your neurosurgeon and the rest of the team will go through
a quality assurance process and everyone will review and
confirm the plan before embarking on the actual treatment.
4. Treatment
 You
will then be taken to the actual Gamma Knife Suite where
you will be allowed to lie down in a comfortable position
(fig. 5). The head frame is now attached to the automatic
position system (APS). This is a very sophisticated computerized
robotic system with high accuracy. At this point, you
may move your arms and legs, but your head will actually
be fixed. All of this will be explained by the nurses
and doctors once inside the unit.
You
will then be taken to the actual Gamma Knife Suite where
you will be allowed to lie down in a comfortable position
(fig. 5). The head frame is now attached to the automatic
position system (APS). This is a very sophisticated computerized
robotic system with high accuracy. At this point, you
may move your arms and legs, but your head will actually
be fixed. All of this will be explained by the nurses
and doctors once inside the unit.
The treatment itself
is silent, completely painless and lasts roughly 30 minutes.
Patients can even bring their favorite CD so they can
listen to their music during the treatment. Some prefer
to sleep through the procedure, and in this case a mild
sedative is given just before the procedure if needed.
The treatment is completely monitored by the team via
a camera in the treatment room. A nurse is also just outside
the room who can see the treatment room on a video screen
and communicate with the patient by microphone. Once the
treatment is completed, you will be allowed to walk back
to the patient suite accompanied by a nurse. The frame
is removed, again with very minimal discomfort, and a
dressing is placed. You will be given another half-hour
or hour to completely recover depending on the amount
of sedation. Once you have completely recovered and are
ready to go home, you will be discharged. Gamma Knife
is generally an outpatient procedure.
Important
Reminders About Gamma Knife
1) Generally you
will not be put to sleep, but you must have nothing to
eat or drink after midnight on the night before the procedure.
You may resume your usual diet after surgery.
2) If you are taking
any blood thinners such as aspirin, Plavix, Coumadin or
any
other such medications, please inform your physician so
that they can be withheld with appropriate approval from
your primary care physician prior to the procedure.
3) Keep pin sites
clean with alcohol the day after the procedure.
4) You may shower
the next day without restriction.
5) There may be some
swelling around the pin sites to which ice can be applied.
6) Medications taken
for trigeminal neuralgia may be continued as before.
Going
Home and Results
While some experience immediate relief with gamma knife,
the majority of patients take six to eight weeks to notice
major improvement in the trigeminal neuralgia pain. As
the pain decreases, you will be encouraged to gradually
wean yourself off the medication after discussion with
your physician.
Regular follow-up
is very important, and you will be given an appointment
to follow up in the office usually six to eight weeks
after the procedure. The first follow-up scan will be
done in about six months to view the radiographic effect
of this treatment. If you are coming from out-of-town,
it is important to obtain the MRI’s or have them
sent to your neurosurgeon for his review.
It is very important
to keep your follow-up appointments. If you do not come
to these appointments and you cannot be located, we will
have to consider your treatment a failure even if you
are well. Please notify us of any address or phone number
changes. We may want to contact you even after your regular
follow-up visit to keep appropriate statistics about long-term
results. Please consider sending us a yearly letter or
postcard to let us know how you are doing.
Out-of-Town
Patients
Gamma Knife Treatment
for Trigeminal Neuralgia is usually done as an outpatient
procedure, and patients do not need to be admitted to
the hospital. For out-of-town patients, we have special
discounted rates with area hotels for which information
is available upon request.
MICROVASCULAR
DECOMPRESSION
Microvascular Decompression (MVD), which is considered
the most invasive form of surgical treatment for Trigeminal
Neuralgia isalso the procedure with the highest success
rate. Since this is an invasive procedure, it is reserved
for a small subsection of patients. Patients who are in
generally good health without major medical problems may
be considered for Microvascular Decompression. Microvascular
Decompression is also offered to patients who may have
failed the less invasive procedures such as Trigeminal
Glycerol Rhizolysis and Gamma Knife Treatment.
As mentioned in the
introduction to this booklet, vascular compression of
the Trigeminal Nerve or fifth cranial nerve is thought
to be the culprit for this painful syndrome in a significant
number of Trigeminal Neuralgia patients. Compression of
the nerve is usually by a blood vessel although very rarely
compression could also be from a tumor or some other vascular
abnormality (fig. 6)
Preoperative
Planning
Remember to inform your doctor if you have any specific
allergies. If you are on aspirin, Coumadin, Plavix, or
any other blood thinners, be sure that you have informed
your doctor and discontinued these medications with appropriate
approval for at least a few days prior to the operation.
On the eve of your operation, make sure you have showered
and shampooed your hair very thoroughly without applying
any sort of spray, mousse, gel or any other such material.
A small portion of hair behind the ear will have to be
shaved for the operation, and it is best not to have applied
any greasy or oily material and to have the hair in its
cleanest, natural form for this. You will need to make
a list of all the medications you have been taking at
home to provide to your physician. You will have to sign
a consent form for the operation which will include consent
for a blood transfusion. It is extremely rare for blood
to be used for these surgeries, but permission is obtained
in case of an extremely unexpected emergency situation.
You may discuss this matter with your surgeon ahead of
time if you have any specific concerns about this matter.
You will be advised
not to eat or drink after midnight, and it is best to
stay on
a very light and liquid diet for the entire
day before the operation. Blood pressure medications should
not be withheld, but no blood thinners such as aspirin,
Plavix or Coumadin should be taken for a few days prior
to the operation. If you are on blood pressure medications
or other cardiac medications other than blood thinners,
it is usually advisable to take this with a sip of water.
Any herbal medications such as garlic pills, fish oil,
etc., be sure to inform your surgeon. Most likely you
will be asked to stop those for a few days before your
operation as well.
The
Surgical Procedure
Unlike the other procedures, Microvascular Decompression
requires general anesthesia which means this is done in
the operating room with you completely unconscious and
the anesthesiologist monitoring you throughout the operation.
A small incision will be made behind the ear (fig. 7)
on the same side as the trigeminal neuralgia pain. The
incision is carried down through the skull and a very
small hole is made as a window to approach this blood
vessel. The covering of the brain, called the dura, is
opened, and medications are usually given to allow the
brain to relax so that the surgeon can work through a
very small angle under microscopic magnification to expose
the nerve. Once the nerve is exposed and particularly
when its entrance to the brain stem is seen, a careful
inspection is done for vascular compression. After detecting
the vascular compression, the surgeon will elevate the
blood vessel off of the nerve and place pledgelets of
Teflon (fig. 8). The Teflon material is synthetic and
is easily placed between the nerve and the vessel. This
creates a partition between the nerve and the vessel so
that the vessel no longer pulsates on the brain stem.
Closure is done by suturing the dura and placing a synthetic
material to cover the hole made in the bone. Upon completion,
there is no defect in the bone and the incision will heal
very nicely.
Once the surgery
is complete, you will be transferred to the recovery room.
The surgeon will then explain the results to your family
in the waiting room and you will be transferred to the
Neuroscience Intensive Care Unit (NICU).
Usually you will
spend one night in the Neuroscience Intensive Care Unit
with mobilization the following day out of ICU to a regular
private room. On the first day after surgery, you will
usually be allowed to get out of bed and have breakfast.
The dressing will not be changed for three days. On the
second or third day, the patient is discharged after dressing
change.
Results
The results of Microvascular Decompression are usually
very good, and there is usually a much lower recurrence
rate than with other procedures. However, this is a major
surgical intervention, and the potential for complications
is also much higher compared to less invasive procedures
of Trigeminal Glycerol Rhizolysis and Gamma Knife Treatment.
Since this is an open operation, it does carry the potential
complications that come with general anesthesia. At the
same time, other potential risks of open procedure such
as hemorrhage, stroke, loss of function of certain cranial
nerves - specifically loss of hearing in a very small
percentage of patients - must be given consideration.
In experienced hands,
this surgery has very good results, but even in the best
of hands major complications can occur, and details should
be thoroughly discussed with your surgeon. Whenever Microvascular
Decompression is offered, your surgeon will sit down with
you and your family members and go over the entire protocol
of the operation with thorough discussion of the risks
and benefits. Ample opportunity will be provided for you
and your family to ask and receive satisfactory answers
to questions.
Discharge
Planning
Once you are discharged, you will be advised to keep your
head elevated on two or three pillows for at least two
to three weeks. You will usually be instructed not to
get your incision wet until return to the surgeon’s
office for removal of the stitches and dressing change.
During the first seven to ten days, you must refrain from
any strenuous activities such as lifting, bending or for
that matter even driving. After ten days and having seen
the surgeon in the office for the first follow-up visit,
you are usually allowed to return to normal activities.
We usually instruct
patients to stay very active after the operation and encourage
you to start moving as soon as you are stable and regain
complete balance. It is very important to keep in mind
that while the patient is in the bed and not ambulating,
the blood can pool in the leg and lead to blood clots
in the legs, which can be very dangerous. To prevent this
during the operation and your stay in the intensive care
unit, special stockings are used which cause intermittent
massage and compression of the legs. This helps to prevent
the formation of any blood clots in the leg. Once you
are transferred to a regular room and after you are discharged
home, you should continue to wear TED hose stockings until
you are very active with ambulation and no longer need
the elastic hose. It is very important for smokers to
quit smoking several days before the operation. Deep breathing
and gentle coughing exercises after surgery are also very
important to keep your lungs moving and prevent pneumonia.
Usually a nurse and the respiratory therapist will help
to educate you on specific exercises during your hospital
stay. Elderly patients and smokers are especially encouraged
to
continue these exercises at home.
If you notice any
leakage of fluid through the nose or back of the throat,
you should immediately alert your surgeon, as this could
be a sign of spinal fluid leakage from the surgery. If
you experience fever, headache, nausea, vomiting, neck
stiffness or any such problems, the surgeon should also
be promptly informed. Most patients are taken off of anticonvulsants
rather quickly after this operation unless you have been
on the medication for a very long time in which case you
will be gradually tapered off.
Final
Decision
Dr. K. Singh Sahni spends a lot of time discussing each
individual procedure with his patients and family members.
The final decision
to select the surgical procedure is made by the patient
while Dr. Sahni helps them with this process.
You should feel comfortable
asking any questions during your consultation with Dr.
Sahni. He has a lot of patience and compassion for his
TN patients.
About the
Surgeon
K. Singh Sahni, MD, FACS is a distinguished neurosurgeon
with a special interest in the treatment of trigeminal
neuralgia. Over the last twenty years, he has treated
close to 2,000 patients who suffer with facial pain syndromes.
While there are a number of physicians who may offer one
or the other preferred methods of treatment for trigeminal
neuralgia, as one who subspecializes in this disease Dr.
Sahni has expertise in all methods of treatment, surgical
and nonsurgical. This enables him to tailor each patient’s
treatment based on the patient’s age, general medical
condition and overall manifestation of pain. All of this
affords the best-case scenario for the trigeminal neuralgia
patient of having the opportunity to work with a neurosurgeon
who is able to offer all treatment options at the same
facility with a single physician without bias toward a
specific procedure. Dr. Sahni is a board certified Neurosurgeon.
He is the Medical director of Gamma Knife Unit. He obtained
his GK training in Stockholm, Sweden. Dr. Sahni has been
performing TGR (Glycerol injections) and MVD (Microvasular
Decompression) for over twenty years.
Glossary
of unfamiliar terms
Aplastic anemia: Low white blood cell
count caused by decreased bone marrow function.
Bilateral: Two-sided.
Dura: The covering of the brain.
Fifth cranial nerve: Cranial nerve that
serves the face, teeth, mouth and nose. Same as trigeminal
nerve.
GK: Gamma Knife
Intractable: Resistant to cure, relief
or control.
Mandibular: Related to the lower jaw.
Maxillary: Related to the upper jaw.
MVD: Microvascular Decompression
Ophthalmic: Related to the eye.
Refractory: Resistant to treatment.
Root entry zone: The region very close
to the brain stem, especially where the trigeminal nerve
originates.
TGR: Trigeminal Glyerol Rhizolysis
Tic douloureus: Painful condition characterized
by severe, excruciating, episodic face pain. Same as trigeminal
neuralgia.
Trigeminal nerve: Cranial nerve that
serves the face, teeth, mouth and nose.
back
to the top >